Body Dysmorphia, also referred to as Body Dysmorphic Disorder (BDD), is a mental health condition in which patients stress about supposed imperfections in their physical appearance. This is a complicated disorder that goes much beyond appearance issues. Even though the suffering person has uncontrolled thoughts dominated by these apparent flaws, which are frequently invisible to others, they cause distress and interfere with daily activities.
Furthermore, it can impact a person’s social and professional relationships and mental health.
Mental health conditions are highly misunderstood and people still feel weird about talking openly about it, therefore, awareness regarding brain health and its impact on overall wellbeing is greatly needed and important.
What is body dysmorphic disorder?

Body dysmorphia is a psychological disorder with profound roots that goes beyond simple dissatisfaction with one’s looks. BDD sufferers focus their attention on one or more physical characteristics, such as their complexion, hair, nose, or body shape, that they believe to be imperfect. They could avoid social situations out of dread of being judged, spend hours examining their reflection, or ask for assurance from others. Significant mental health issues, such as anxiety, depression, and social isolation, can result from this illness.
According to the DSM-5-TR, Body Dysmorphia is a serious disorder that creates a great deal of mental pain and behavioral patterns, such as repetitive activities, social scenario avoidance, and even suicidal thoughts. It is not only self-importance. Education regarding its identification and treatment is crucial because it is often misunderstood and under-recognized.
Furthermore, Body Dysmorphic Disorder (BDD), which presents as an obsessive fixation on alleged physical defects that are frequently invisible to others, is the perfect example of how psychological perception and physical reality run into. This crippling Body dysmorphic condition represents significant changes in cognitive and emotional processing, impacted by genetic inclinations, neurobiological abnormalities, and environmental stressors. It is not only a sign of self-importance or self-consciousness.
The Body Dysmorphia condition is made worse by the widespread influence of social media and cultural beauty standards, which feed cycles of self-criticism and outside approval. Clinically, Body dysmorphic disorder necessitates a complex treatment strategy that combines evidence-based treatments like medication and Cognitive Behavioral Therapy (CBT) with larger social initiatives to undo damaging beauty standards.
Simply put, an obsession with physical appearance, typically centered on a perceived fault that may not exist or is exaggerated in the person’s perception, is a feature of Body dysmorphic disorder. For people with BDD, their perceived flaws frequently take center stage in their lives, leading to:
Extreme distress
- Disturbance of day-to-day tasks
- Repetitive behaviors such as plucking at one’s skin, compulsive grooming, or needing constant reassurance
Important attributes:
People frequently seem “normal” to others.
This obsession may result in repeated, needless cosmetic or surgical procedures that rarely ease their suffering.
Body dysmorphic disorder has many different and complicated original causes. They frequently involve a convergence of circumstantial factors like bullying or cultural beauty standards, personality traits like perfectionism, brain chemistry, and genetic predisposition.
Nonetheless, certain aspects of BDD are concerning. Although BDD can affect any part of the body, the following are characteristic areas of the center:
- Skin, nose, eyes, lips, or ears are examples of facial features.
- Thighs, stomach general shape of the body like worrying about symmetry, size, or proportion.
- Although BDD is a difficult disorder, people can get the care they require if they are aware of its signs and areas of concern.
Behaviors and Symptoms of Body Dysmorphia
People who suffer from body dysmorphia often show diverse symptoms and actions that are indicative of their strong obsession with appearance.
Individuals who suffer from Body Dysmorphic Disorder (BDD) may take extreme measures to conceal their apparent flaws like spending a major time on personal grooming, including hair styling, cosmetics application, and outfit selection.
Furthermore, the sufferers are;
- Always contemplating perceived shortcomings for hours each day
- Asking loved ones if they look okay over and over again, yet never trusting their responses.
- Exercising excessively or adhering to severe diets in an attempt to “fix” their perceived flaws.
- Sometimes they won’t leave the house because they don’t want their imperfections to be seen.
- Mental health issues are also associated with Body dysmorphia feeling depressed, anxious, or even considering suicide.
- Skin-picking, obsessive grooming, or frequent mirror-checking are examples of compulsive behaviors.
- Having obsessive thoughts like Worrying about one’s appearance all the time.
- Seeking approval and constantly seeking affirmation from others on one’s appearance.
- Doing Comparisons and assessing against others results in inferiority complexes for sufferers.
- Having an obsession with cosmetic surgery like Seeking dermatological procedures or treatments that experts consider unneeded. Some people have the same location operated on more than once.
- Avoidance tactics include avoiding mirrors completely or refusing to snap pictures.
These actions are motivated by severe psychological suffering. If untreated, they can worsen and affect work, relationships, and general quality of life.
The Impact of Body Dysmorphia on Day-to-Day Living
Beyond just its effects on mental health, body dysmorphia can seriously impair a person’s ability to go about their everyday life. Because of their obsessions and fears, many people with Body dysmorphic disorder find it difficult to keep relationships or find stable work. Social gatherings can become intolerable, which can cause loneliness and hideaway.
Additionally, because people frequently look for cosmetic surgeries or products to “fix” their perceived imperfections, the illness can lead to financial distress. Regretfully, these attempts rarely calm their worries and may even make them worse.
Furthermore, Social media and contemporary culture have a big influence on how people see themselves. Through filters, editing tools, and carefully chosen content, platforms such as Instagram and TikTok frequently propagate unachievable beauty ideals. This constant exposure can worsen self-doubt and feelings of inadequacy, especially in sensitive people.
The emergence of influencer culture has increased social pressure to adhere to particular standards of beauty. To comprehend and lessen the wider effects of BDD, it is imperative to address these outside factors.
Similarities Between Body Dysmorphic Disorder (BDD) and Other Conditions
The diagnosis of body dysmorphic disorder (BDD) can occasionally be made more difficult by the fact that it has characteristics with many other psychological disorders. It is easier to distinguish BDD from related disorders when these similarities are understood:
Due to its overlap with other diseases, BDD is commonly misdiagnosed.
Obsessive-compulsive disorder, or OCD, is characterized by compulsive thoughts and behaviors.
Similar avoidance tendencies are seen in social anxiety disorder.
Depression or Agoraphobia: BDD is frequently characterized by emotional detachment and loneliness.
Patients may first turn to dermatologists, cosmetic surgeons, or general practitioners for assistance, concentrating only on the outward manifestation of their perceived shortcomings rather than mental health professionals.
OCD, or obsessive-compulsive disorder
BDD includes activities intended to “fix” perceived imperfections (compulsions) and unwanted, periodic thoughts about appearance (obsessions). Due to these characteristics, Body dysmorphic disorder and OCD are quite similar, and some specialists view BDD as a subtype of OCD. In real life, a lot of people with BDD diagnoses may also have a history of OCD.
Fear of Social Situations
When avoidance behaviors are motivated by worries about appearance, social phobia which is an anxiety disorder characterized by a fear of social interaction shares traits with BDD. For example, a person with BDD can shy away from social situations out of dread of being ridiculed or judged for their perceived shortcomings.
Agoraphobia
Agoraphobia is characterized by a fear of being in circumstances from which one feels unable to flee, which frequently leads to a person remaining at home. Instead of agoraphobia itself, people with Body dysmorphic disorder may isolate themselves because they are afraid of showing their perceived flaws.
Anorexia Nervosa
Although the focus is different, both BDD and anorexia nervosa involve an extreme obsession with appearance. BDD involves an obsession with particular physical characteristics, whereas anorexia nervosa is focused on regulating body weight and shape. Nonetheless, the two may coexist; some people may have both illnesses at the same time.
Hypochondriasis
Body dysmorphic disorder concentrates on perceived physical flaws, whereas hypochondriasis involves compulsive worries about getting a catastrophic illness. Both conditions share a pattern of excessive concern that takes over the person’s thinking, despite the differences in the concerns.
Trichotillomania
When compulsive hair-pulling, or trichotillomania, is motivated by unhappiness with one’s looks, it might resemble Body dysmorphic disorder. Similarly, the compulsive behaviors observed in trichotillomania are mirrored in BDD, when hours are spent picking at or pinching skin imperfections.
Clinicians can ensure that people with BDD receive the particular care they require by accurately diagnosing them and developing customized therapies by being aware of these parallels.
Causes for Body Dysmorphic disorder
Several biological, social, and psychological elements contribute to the development of body dysmorphic disorder (BDD). Although this field’s research is still in its beginning, the following are the main conclusions:
Biological Factors: Research has linked a gene associated with GABA-A receptors to BDD, indicating a hereditary component.
According to twin research, genetic factors may be responsible for 43% of BDD cases.
Social and Psychological Factors:
BDD is more likely to develop after traumatic events like physical or sexual abuse.
BDD is more common in people who experienced parental neglect or a lack of attention as children.
Epidemiology: BDD Affects Who?
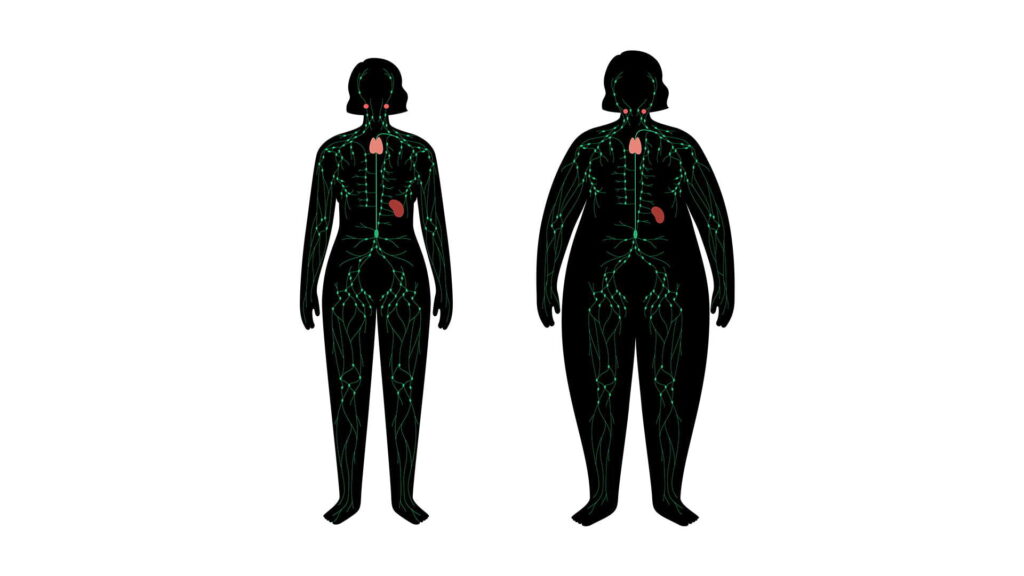
Body Dysmorphia is a worldwide disorder that affects people of all ages, with a somewhat higher prevalence among women. The statistics are as follows:
Global Prevalence:
- 2–3% in adulthood
- 2–5% in teenagers
- 3% of college students
In Health Care Settings:
- BDD affects about 13% of patients at cosmetic surgery clinics.
- In some operations, the frequency is significantly higher:
- 20% are rhinoplasty (nose surgery).
- 11% had jaw surgery.
- Dental correction or orthodontics: 5–10%.
Numerous mental illnesses, such as eating disorders, bipolar disorders, anxiety, depression, and OCD, frequently coexist with BDD.
DSM-5-TR Diagnostic Criteria for Body dysmorphic disorder
The following requirements must be fulfilled to diagnose Body Dysmorphia:
Preoccupation with Appearance: Constantly thinking about alleged imperfections that are invisible or seem insignificant to other people.
Repetitive behaviors that are motivated by obsession include obsessive grooming, mirror-checking, and skin-picking.
Significant Distress: The fixation interferes with social, professional, or other sides of everyday life and produces unbearable emotional distress.
Not More Suitable for Another Disorder: For example, eating disorder-related worries about body fat.
Efficient Diagnosis and Screening
To better identify BDD, physicians ought to:
Make use of screening instruments with proven results, such as the Body Dysmorphic Disorder Questionnaire (BDDQ).
Watch out for people who want frequent dermatological or cosmetic operations.
Focus on the patient’s emotional reaction to their look during organized interviews.
Keep an eye out for functional deficits and repetitive habits, such as avoiding social situations, employment, or school.
Methods of Treatment Based on Evidence
An interdisciplinary strategy is necessary to manage BDD, combining:
Combating negative thought patterns is the main goal of cognitive-behavioral therapy or CBT.
Pharmacological Treatment: To treat anxiety and compulsive thinking, doctors frequently prescribe selective serotonin reuptake inhibitors or SSRIs.
Collaborative Care: Involve mental health specialists, dermatologists, and cosmetic surgeons to inform patients about the pointlessness of surgical remedies and to concentrate on psychological therapies.
Support Systems: Involving peers and family is essential to lowering stigma and enhancing therapeutic compliance.
Impact on Behavior and Emotions
Significant emotional distress results from the continual conviction that one is unpleasant or disproportionate. Patients resort to repetitive activities, also referred to as rituals or compulsions, as a coping mechanism. These actions are intended to relieve the mental stress brought on by their compulsive thoughts.
Ritual Examples:
Physical: Exercise, excessive grooming, hiding, and checking the mirror.
Mental: Self-reassuring, counting, and comparing one to others.
Adaptive: Frequently switching outfits or hiding perceived imperfections.
At some point, all Body dysmorphic disorder individuals exhibit repetitive behaviors, notwithstanding differing degrees of visibility. Others might not notice certain rituals, such as mental comparisons or internal self-assurance.
Observable Patterns and Results
During patient contacts, practitioners may observe tangible evidence or direct behaviors:
Skin injuries or scarring from picking are visible indicators.
Damage or loss of hair as a result of excessive grooming.
Patients may actively participate in actions such as vocalizing complaints, examining faults, or combing their hair.
Assessment of Mental Status
The degree of a patient’s obsession is frequently revealed during a mental health assessment. This procedure can:
Differentiate between a real physical problem and a perceived flaw.
Emphasize the psychological and emotional toll that these obsessions take.
Provide details on the particular issues at hand.
When a physical examination is conducted, it should focus on the patient’s stated areas of concern to distinguish between perception and reality.
Nonetheless, Body dysmorphia is usually effectively treated with a mix of support networks and therapy. The gold standard is cognitive behavioral therapy (CBT), which assists people in overcoming maladaptive thought patterns and creating more constructive coping strategies. To treat related anxiety or depression, doctors may occasionally prescribe drugs such as selective serotonin reuptake inhibitors (SSRIs).
Open communication and support groups can also be highly important for healing. People with BDD frequently get validation and reassurance that they are not alone in their challenges by sharing their experiences. To offer sympathetic and helpful assistance, family members and friends should be informed about the disorder.